Correlates of Protein Intake Among Community Dwelling Older Adults
Meredith E. Sargent and Kelly L. Evola
G. Kevin Randall*
Jeannette Davidson*
Bradley University
Abstract
KEYWORDS: protein intake, older adults, life regard
Nutritional recommendations, BMI, and quality of life may be uniquely related in a population of older adults. The current recommended dietary allowance (RDA) for dietary protein in older adults is 0.8 g/ kg of body weight per day, but controversy exists as to whether this amount is adequate. Research findings suggest that the protein turnover rate decreases by the age of 70, resulting in a greater need for protein by older adults. In addition, nutritional studies have suggested a lower mortality rate is associated with overweight BMI ranges in older adults. Last, a relationship between nutritional risk and quality of life has been found in community living elderly adults. To date no studies have been found investigating the relationship between protein intake and various physical and mental health correlates, such as quality of life among community dwelling older adults. Using data collected from a convenience sample of this population, who indicated protein intake of 0.8 -1.6 g/kg and BMIs of 25 and over, we investigated the relationship between protein intake, self-rated physical health, and life regard; analyses controlled for age, sex, and marital status. Results from a hierarchical regression analysis showed that a measure of life regard significantly and positively contributed to Protein Intake. This final model explained 49 percent of the variance.
Multiple changes occur within the body as people age, often with harmful outcomes. Perhaps one of the most evident changes is a loss of skeletal muscle due to a decrease in total body protein that can lead to muscle weakness, falls, and injuries (Chernoff, 2004). This decrease in total body protein also results in a decrease of organ tissue, blood components, and immune system cells. These results can have serious implications including impaired wound healing, decreased skin elasticity, and decreased immune function (Chernoff). It is imperative that older adults meet their protein and energy needs. Without adequate protein intake, the body can adjust, but the result may be muscle mass loss, decreased ability to perform life tasks, and depressed immune function (Chernoff). The ability to perform everyday tasks is especially important to community dwelling older adults as they must be able to take care of themselves and be independent, resulting in higher levels of perceived quality of life (Houston et al., 2008).
The current recommended dietary allowance (RDA) for dietary protein intake in older adults is 0.8 g/ kg of body weight per day, but there is some controversy as to whether this amount is adequate. Chernoff (2004) suggested that the protein turnover rate decreases by the age of 70 and therefore, more dietary protein is needed to replace lost protein, but this recommendation is still in question because the current RDA maintains nitrogen balance in the short term. However, the body may adjust by using muscle protein over a longer period of time (Houston et al., 2008). Other researchers have investigated the effects of high protein intake. A study by Walrand and colleagues (2008) assessed the effect of a high protein diet consisting of 3.0 g of protein per kg of lean muscle mass in older adults as compared to younger adults and found no positive effects on muscle protein synthesis in either population, but did find a major difference in glomerular filtration rate between older adults and younger ones, suggesting that a high protein diet may be a concern for older adults.
Although previous cross-sectional studies have failed to find a significant association between protein intake and lean muscle mass in community dwelling older adults (Baumgartner, Walters, Gallagher, Morley, & Gary, 1999; Mitchell, Haan, Stenberg, & Visser, 2003), a longitudinal study by Houston et al. (2008) suggested that protein intake may be a changeable risk factor for muscle loss in older adults. Their research revealed that older adults who consumed the most protein maintained more lean body mass after three years than did those who consumed the least.
Recent studies have suggested that a lower mortality rate is associated with overweight BMI ranges in older adults (Diehr, et al., 2008; Stessman, Jacobs, & Bursztyn, 2009). Stessman et al. focused on examining the relationship between BMI and mortality rates over an eighteen year time period, in which older adults born in 1920/21 were followed up from ages 70 to 88 years. Results showed that a greater BMI value was associated with lower mortality throughout the follow-ups across this age range. Similar conclusions were reached by Heiat, Vaccarino, and Krumholz (2001) in a systematic review. Based on mortality, they found that the ideal BMI is higher for older adults. More specifically, this applied to older adults over the age of 65 with BMI’s falling in the “overweight” range from 27-30.
Research has also demonstrated that there is a relationship between nutritional risk and quality of life among community living older adults (Keller, Ostbye, & Goy, 2004). In nursing home patients, the Quality Nutrition Outcomes-Long Term Care Model (QNO-LTC) has been utilized to investigate protein-calorie malnutrition, BMI, and functional status (Crogan & Pasvogel, 2003). To date no studies have been found investigating the relationship between protein intake as a percentage of RDA and quality of life in community-dwelling older adults.
The QNO-LTC model suggests that psychiatric and mood disorders, older age, and decreased ability to perform ADLs may be predictors of nutritional status and that nutrition status could then influence long term outcomes such as perceived quality of life, functional status, depression, and psychosocial well-being (Mitchell, Ferketich, & Jennings, 1998). This model was used as a guide for our study. We applied the model to the community dwelling older adult population and used protein intake as a marker of nutritional status as the study’s outcome with other correlates as predictor variables. Thus, the purpose of the current study was to investigate the relationship between known correlates (e.g., age, sex, marital status, self-reported physical health, and quality of life) and protein intake among community dwelling older adults who reported 100-200 percent RDA protein intake and had assessed BMI greater than or equal to 25. Specifically, based on the research performed by Houston and colleagues (2008) and the QNO-LTC, we hypothesized that there would be a significant correlation between protein intake and quality of life after accounting for the influence of the other known correlates.
Method
Sample and Procedures
The dietary and psycho-social data reported is from Bradley’s Health and Aging Study. This study, approved by the University’s Committee on the Use of Human Subjects in Research, was a cross-sectional study of 145 independent, community dwelling older adults in the Midwest, 60 years and older (60-69 years, n =16; 70-79 years, n = 48; and 80-98, n =36). During a 2-hour, private, in person interview, conducted by trained research assistants, demographic, psychosocial, dietary, nutritional, health, physical ability and cognitive assessments, and anthropometric measurements were obtained. Of this sample, 72 percent were female, the average age was 77 (SD = 6.7), 79 percent were White, 38 percent were married, and 53 percent reported completing more than high school.
Measures and Data Analysis
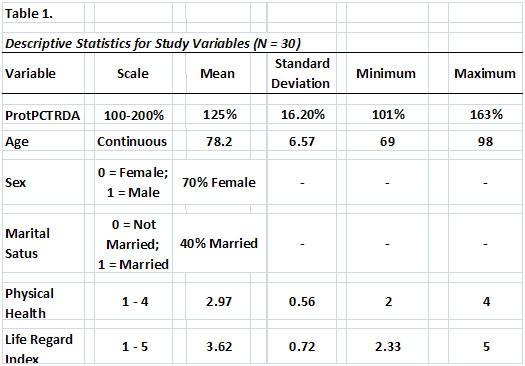
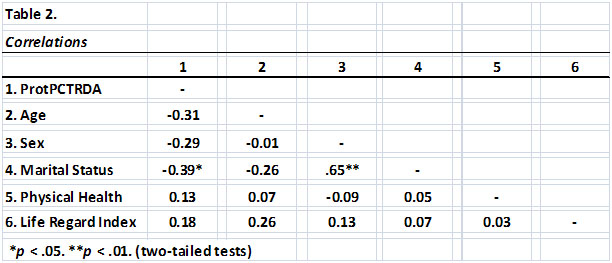
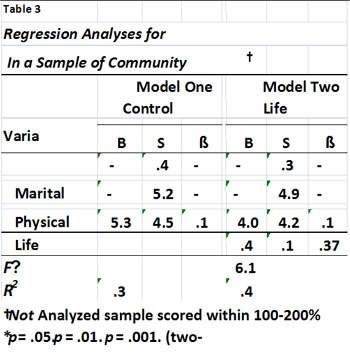
Table 1 provides the measurement scale and descriptive statistics (mean, standard deviation, minimum and maximum) for each of the study’s variables. A 24-hour diet recall was conducted using a three-pass method to obtain food intake information, in particular for this study, Protein as a percentage of recommended dietary allowance (ProtPCTRDA). Diet analysis of protein intake was analyzed for 87 participants using The Food Processor (Food Processor, 2005) to determine our outcome variable, percent protein of RDA (ProtPCTRDA). Participants responded to a single question assessing their self-reported Physical Health. Research has validated a single-item measure of self-rated physical health as a summary assessment of overall health status, predictive of various outcomes (Jylhä, Volpato, & Guralnik, 2006; Rohrer, Herman, Merry, Naessens, & Houston, 2009). Following the suggestions in the literature regarding the Life Regard Index (LRI; Debats, 1998; Harris & Standard, 2001; Steger, 2007), we employed the adjusted version but retained the original 5-point Likert-scale where 1 = disagree to 5 = agree. In addition, in our sample of older adults (N=147), the two subscales (i.e., fulfillment and framework) were highly and significantly correlated (r = .83; p < .001). Thus, we used the entire scale of 28 items (Harris & Standard), which had internal consistency of alpha = .87; our dependent or criterion variable was an overall average of the participant’s score on the LRI. Descriptive statistics and all other analyses were conducted using SPSS (SPSS Inc., IL, version 15.0, 2007). Pearson correlation coefficients were calculated for the zero-order correlations (see Table 2) and hierarchical multiple regression was performed to answer the study’s hypotheses (see Table 3).
Results
After examining descriptive statistics (see Table 1) for the study’s analyzed sample (N=30) of those participants who scored within 100-200 percent RDA protein and had BMI greater than or equal to 25.0, we calculated zero order correlations for all study variables (see Table 2). Protein as a percentage of RDA was significantly and negatively correlated with age, sex (0=female; 1 = male), and marital status (0 = not married; 1 = married) and approached statistical significance with the Life Regard Index (r = .22; p < .10, for a two-tailed test). Based on these encouraging results, we conducted a hierarchical regression analysis for predictors of protein intake, or ProtPCTRDA, with two blocks of predictors. The first block included the control variables, age, marital status, and physical health. The final block included our predictor of interest, Life Regard Index (see Table 3). In Model 1, the block of control variables significantly predicted the outcome, explaining 37 percent of the variance; only Physical Health was not a significant predictor or control (β = .18; p >.05). The final model added the psychosocial predictor, Life Regard Index, an assessment of meaning in life. This scale significantly and positively contributed to Protein Intake (F∆ = 6.19; p < .05). This final model explained 49 percent of the variance. Thus, controlling for the influence of age, marital status, and physical health, meaning in life, as assessed by the Life Regard Index, significantly contributed to participants’ protein intake.
We did assess our models for possible violations of the assumptions of ordinary least squares regression. First, histograms and scatter plots of standardized predicted values and standardized residuals appeared normally distributed and randomly scattered (homoscedasticity); the Durbin-Watson statistic was 2.35 (independent errors). Second, we checked for multicollinearity using the tolerance statistic and Menard’s (1995) suggestion that values below .2 are suspect; tolerances in our analysis ranged from .89 to .99. And last, we assessed the undue influence of individual cases based on Cook’s Distance greater than 1.00 (Field, 2009; Stevens, 2002). The average Cook’s Distance was .04; the minimum was .00 and the maximum was .19. Thus, we are fairly confident that our reported results are robust to possible violations of the analyses assumptions.
Discussion
The purpose of the current study was to investigate aspects of the long-term outcomes portion of the Quality Nutrition Outcomes-Long-term Care Model (Houston et al., 2008; Mitchell, Ferketich, & Jennings, 1998) among community dwelling older adults. Specifically, based on the research performed by Houston and colleagues and the QNO-LTC, we hypothesized that there would be a significant correlation between protein intake and quality of life, assessed by the Life Regard Index, after accounting for the influence of known correlates. Our results confirmed this relationship in a sample of older adults who reported protein intake within 100-200 percent RDA and had BMI assessed at 25 or greater.
The study’s results add to that of others regarding higher BMIs, adequate protein intake, and quality of life for older adults. However, because the data were cross-sectional and limited in sample size, the study’s findings in general are suggestive only and the direction of influence among the variables cannot be determined. Possibly, factors influencing meaning in life could be malleable tools for improving protein intake in this population. Or, it could be that nutritional interventions to increase protein in participants’ diets may well increase life regard. Although the maxim, correlation does not prove causation, is well heeded in this case, so also is the fact that without association, there is not causation. Thus, the results of the present study encourage further investigation into this empirical link between quality of life and a specific aspect of nutritional status, protein intake.
Erikson (1998) highlighted the salience of successfully mastering challenges of psychosocial stages throughout life. Reviewing and recognizing the importance of Erikson’s stages and challenges, such as identity vs. identity confusion and generativity vs. self absorption, may very well increase one’s life regard and also influence adequate protein intake. Investigating what mechanisms possibly link these two is grounds for future research. For example, having a good sense of one’s self in later stages of life and feeling like a productive member of society with a purpose may positively influence both one’s outlook on life and the protein in one’s diet. However, the direction of influence may well be in the other direction: it may be that having adequate or greater protein intake is a proxy for good health and social relationships both of which may increase one’s sense of life satisfaction.
In order to determine a more direct relationship between life regard and protein intake in community dwelling older adults, future research should increase the sample size and consider an experimental design to clarify the present study’s findings. Increased specificity of diet recalls with regard to types of food consumed and portion sizes would yield a more accurate measure of protein intake. These minor adjustments would make for a more direct portrayal of the relationship between life regard and protein intake in community dwelling older adults, perhaps adding life to years.
References
Baumgartner, R. N., Walters, D. L., Gallagher, D., Morley, J. E., & Gary, P. J. (1999). Predictors of skeletal muscle mass in elderly men and women. Mechanisms of Ageing and Development, 107, 126-136.
Chernoff, R. (2004). Protein and older adults. Journal of the American College of Nutrition, 23, 627S-630S.
Crogan, N. L., & Pasvogel, A. (2003). The influence of protein-calorie malnutrition on quality of life in nursing homes. Journal of Gerontology, 58A, 159-164.
Debats, D. L. (1998). Measurement of personal meaning: The psychometric properties of the Life Regard Index. In P. T. P. Wong & P. S. Fry (Eds.), The human quest for meaning: A handbook of psychological research and clinical applications (pp. 237 – 259). Mahwah, New Jersey: Lawrence Earlbaum Associates, Publishers.
Diehr, P., O’Meara, E. S., Fitzpatrick, A., Newman, A. B., Kuller, L., & Burke, G. (2008). Weight, Mortality, Years of Healthy Life, and Active Life Expectancy in Older Adults, Journal of the American Geriatrics Society, 56(1), 76-83.
Erikson, J. M. (1998). The life cycle completed. New York, NY: W. W. Norton & Company, Inc.
Field, A. (2009). Discovering statistics using SPSS (3rd ed.). Thousand Oaks, CA: Sage.
Food Processor (Version 8.6.0) [Computer software] (2005). Salem, OR: ESHA.
Harris, A. H. S., & Standard, S. (2001). Psychometric properties of the Life Regard Index- Revised: A validation study of a measure of personal meaning. Psychological Reports, 89, 759-773.
Heiat, A., Vaccarino, V., & Krumholz, H. M. (2001). An evidence-based assessment of federal guidelines for overweight and obesity as they apply to elderly persons. Arch Intern Med ,161, 1194-2003.
Houston, D. K., Nicklas, B. J., Ding, J, Harris, T. B., Tylavsky, F. A., Newman, A. B., J. Lee, J. S., Sahyoun, N. R., Visser, M, & Kritchevsky, S. B. (2008). Dietary protein intake is associated with lean mass change in older, community-dwelling adults: The Health, Aging, and Body Composition (Health ABC) Study. The American Journal of Clinical Nutrition, 87, 150-155.
Jylhä, M., Volpato, S., & Guralnik, J. (2006). Self-rated health showed a graded association with frequently used biomarkeers in a large population sample. Journal of Clinical Epidemiology, 59, 465-471.
Keller, H. H., Ostbye, T., & Goy, R. (2004). Nutritional risk predicts quality of life in elderly community-living Canadians. Journal of Gerontology, 59A, 68-74.
Menard, S. (1995). Applied logistic regression analysis. Sage university paper series on the quantitative applications in the social sciences, 7-106. Thousand Oaks, CA: Sage.
Mitchell, D., Haan, M. N., Stenberg, F. M., & Visser, M. (2003). Body composition in the elderly: the influence of nutritional factors and physical activity. Journal of Nutrition, Health and Aging, 7, 130-139.
Mitchell, P., Ferketich, S., & Jennings, B. (1998). Quality health outcomes model. Journal of Nursing Scholarship, 30, 43-46.
Rohrer, J. E., Herman, D. C., Merry, S. P., Naessens, J. M., & Houston, M. S. (2009). Validity of overall self-rated health as an outcome measure in small samples: A pilot study involving a case series. Journal of Evaluation in Clinical Practice, 15, 366-369.
Steger, M. F. (2007). Structural validity of the Life Regard Index. Measurement and Evaluation in Counseling and Development, 40, 97-109.
Stessman, J., Jacobs, J. M., Ein-Mor, E., & Burszytn, B. (2009). Normal Body Mass Index rather than obesity predicts greater mortality in elderly people: The Jerusalem Longitudinal Study. The American Geriatrics Society , 57 (12), 2232-2238.
Stevens, J. P. (2002). Applied multivariate statistics for the social sciences (4th ed.). Hillsdale, NJ: Erlbaum.
Walrand, S., Short, K., Bigelow, M., Sweatt, A., Hutson, S., & Nair, K. S. (2008). Functional impact of high protein intake on healthy elderly people. American Journal of Physiology-Endocrinology and Metabolism, 295, E921-E928.
|